“Veterans Access Expanded for Healthcare: A New Era of Support and Care
Related Articles Veterans Access Expanded for Healthcare: A New Era of Support and Care
- The "Woman Eating Cat" Viral Incident: Unpacking A Disturbing Phenomenon
- Master Security Information Management for Unstoppable Cyber Defense
- X (Twitter) Misinformation Lawsuit: A Deep Dive Into Accountability And Free Speech
- US Sports Highlights: A Season Of Triumphs, Thrills, And Unforgettable Moments
- Mexican Independence Day: A Vibrant Celebration Of Freedom And Heritage
Introduction
On this special occasion, we are happy to review interesting topics related to Veterans Access Expanded for Healthcare: A New Era of Support and Care. Let’s knit interesting information and provide new insights to readers.
Table of Content
Veterans Access Expanded for Healthcare: A New Era of Support and Care
For decades, veterans have faced significant challenges in accessing timely and quality healthcare services. The sacrifices made during their service to the nation often come with physical and mental health consequences that require specialized care. Recognizing the critical need to improve healthcare access for veterans, recent legislative and policy changes have ushered in a new era of expanded access, enhanced services, and improved outcomes. This article delves into the historical context of veterans’ healthcare challenges, the key provisions of expanded access initiatives, the benefits and challenges of these changes, and the future direction of veterans’ healthcare.
Historical Context: The Challenges Veterans Face
Throughout history, veterans have encountered numerous obstacles in accessing the healthcare they need. Long waiting times, bureaucratic hurdles, geographical limitations, and a shortage of specialized providers have plagued the system. These challenges have had profound impacts on veterans’ health and well-being, contributing to higher rates of chronic conditions, mental health disorders, and suicide.
One of the primary factors contributing to these challenges is the complex nature of the Veterans Health Administration (VHA). As the largest integrated healthcare system in the United States, the VHA serves millions of veterans across the country. However, its vast size and intricate structure have often led to inefficiencies, delays, and inconsistencies in care delivery.
Another significant challenge is the growing demand for veterans’ healthcare services. As the veteran population ages and more service members return from conflicts abroad, the VHA has struggled to keep pace with the increasing need for medical care. This has resulted in long waiting lists, limited access to specialists, and difficulties in scheduling appointments.
Furthermore, the unique healthcare needs of veterans often require specialized expertise and resources. Many veterans suffer from service-related injuries, such as traumatic brain injuries (TBIs), post-traumatic stress disorder (PTSD), and musculoskeletal disorders. These conditions necessitate specialized treatment approaches and a comprehensive understanding of the challenges veterans face.
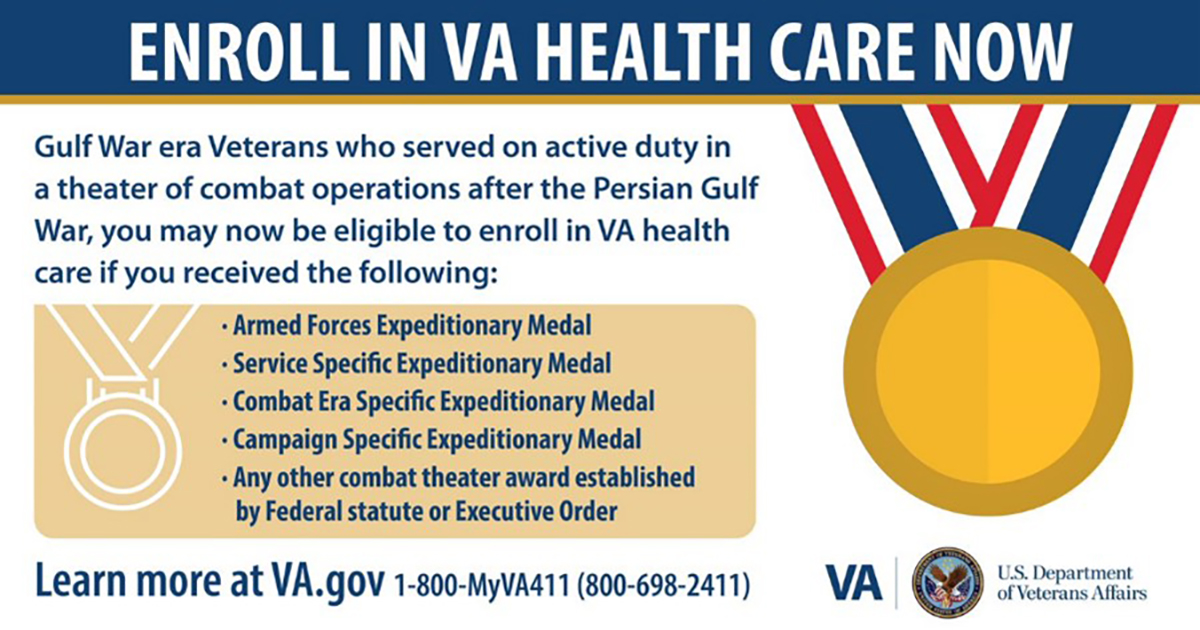
Key Provisions of Expanded Access Initiatives
In response to the persistent challenges in veterans’ healthcare access, Congress and the Department of Veterans Affairs (VA) have implemented several initiatives to expand access and improve the quality of care. These initiatives aim to address the root causes of the problems and provide veterans with more options and flexibility in accessing healthcare services.
One of the most significant pieces of legislation is the Veterans Access, Choice, and Accountability Act (VACAA) of 2014. This law was enacted in response to the 2014 Veterans Health Administration scandal, which revealed widespread delays in healthcare access and manipulation of appointment scheduling. The VACAA aimed to address these issues by expanding veterans’ access to private healthcare providers and increasing accountability within the VA.
Under the VACAA, veterans who meet certain criteria, such as living more than 40 miles from a VA medical facility or facing long waiting times for appointments, are eligible to receive care from private healthcare providers through the Veterans Choice Program (VCP). This program allows veterans to seek care from community-based providers, reducing the burden on the VA system and providing veterans with more convenient access to healthcare services.
In addition to the VACAA, the VA has implemented several other initiatives to expand access to healthcare for veterans. These include:
- Telehealth Services: The VA has expanded its telehealth services, allowing veterans to receive medical care remotely through video conferencing, phone consultations, and mobile apps. Telehealth services are particularly beneficial for veterans who live in rural areas or have difficulty traveling to VA medical facilities.
- Same-Day Services: The VA has implemented same-day services at many of its medical facilities, allowing veterans to receive immediate care for urgent medical needs. This initiative aims to reduce wait times in emergency rooms and provide veterans with timely access to care.
- Community-Based Outpatient Clinics (CBOCs): The VA has established CBOCs in communities across the country to provide veterans with convenient access to primary care, mental health services, and other healthcare services. CBOCs are located closer to veterans’ homes, reducing the need for long-distance travel to VA medical facilities.
- Mobile Vet Centers: The VA operates mobile vet centers that travel to rural and underserved areas to provide veterans with counseling, outreach, and support services. These mobile centers bring healthcare services directly to veterans who may not have access to traditional VA facilities.
- Expansion of Mental Health Services: Recognizing the critical need for mental health services among veterans, the VA has significantly expanded its mental health programs. This includes increasing the number of mental health providers, expanding access to evidence-based therapies, and implementing suicide prevention initiatives.
Benefits of Expanded Access
The expansion of veterans’ healthcare access has yielded numerous benefits for veterans and the healthcare system as a whole. These benefits include:
- Reduced Waiting Times: Expanded access initiatives, such as the Veterans Choice Program and same-day services, have helped to reduce waiting times for appointments and medical procedures. This has allowed veterans to receive timely care and avoid unnecessary delays in treatment.
- Increased Choice and Flexibility: The Veterans Choice Program has provided veterans with more choice and flexibility in accessing healthcare services. Veterans can now choose to receive care from private healthcare providers in their communities, rather than being limited to VA medical facilities.
- Improved Access to Specialized Care: Expanded access initiatives have improved veterans’ access to specialized care, such as mental health services, TBI treatment, and pain management. This has allowed veterans to receive the specialized care they need to address their unique healthcare needs.
- Enhanced Convenience and Accessibility: Telehealth services, CBOCs, and mobile vet centers have enhanced the convenience and accessibility of healthcare services for veterans. These initiatives have brought healthcare services closer to veterans’ homes, reducing the need for long-distance travel and making it easier for veterans to access care.
- Improved Health Outcomes: By providing veterans with timely access to quality healthcare services, expanded access initiatives have contributed to improved health outcomes. Veterans who receive timely and appropriate care are more likely to recover from illnesses and injuries, manage chronic conditions, and maintain their overall health and well-being.
Challenges and Concerns
While the expansion of veterans’ healthcare access has yielded numerous benefits, it has also presented some challenges and concerns. These challenges include:
- Coordination of Care: Coordinating care between VA and private healthcare providers can be challenging, particularly for veterans who receive care from multiple providers. Ensuring seamless communication and information sharing between providers is essential to avoid duplication of services and ensure continuity of care.
- Quality of Care: While the VA has implemented measures to ensure the quality of care provided by private healthcare providers, concerns remain about the consistency and quality of care across different providers. Monitoring and oversight are necessary to ensure that veterans receive high-quality care regardless of where they seek treatment.
- Financial Sustainability: The expansion of veterans’ healthcare access has increased the cost of healthcare for the VA. Ensuring the financial sustainability of these initiatives is crucial to ensure that veterans continue to have access to the care they need in the long term.
- Staffing Shortages: The VA continues to face staffing shortages, particularly in certain specialties and geographic areas. Addressing these shortages is essential to ensure that veterans have access to a sufficient number of qualified healthcare providers.
- Rural Access: While telehealth and mobile vet centers have improved access to healthcare for veterans in rural areas, challenges remain in ensuring that veterans in these areas have access to the full range of healthcare services they need.
The Future of Veterans’ Healthcare
The future of veterans’ healthcare is likely to be shaped by continued efforts to expand access, improve quality, and enhance efficiency. Some of the key trends and developments that are likely to influence the future of veterans’ healthcare include:
- Continued Expansion of Telehealth Services: Telehealth services are likely to play an increasingly important role in veterans’ healthcare, providing veterans with convenient access to care from their homes. Advancements in technology and expanding broadband access will further enhance the capabilities and reach of telehealth services.
- Focus on Preventive Care: The VA is likely to place greater emphasis on preventive care, aiming to prevent illnesses and injuries before they occur. This will involve promoting healthy lifestyles, providing screenings for common health conditions, and offering vaccinations and other preventive services.
- Integration of Mental Health and Primary Care: Recognizing the close relationship between mental and physical health, the VA is likely to further integrate mental health services into primary care settings. This will make it easier for veterans to access mental health care and ensure that their mental health needs are addressed as part of their overall healthcare.
- Use of Data Analytics: The VA is likely to make greater use of data analytics to improve the quality and efficiency of healthcare services. Data analytics can be used to identify trends in healthcare utilization, predict future healthcare needs, and evaluate the effectiveness of different treatment approaches.
- Collaboration with Community Partners: The VA is likely to continue to collaborate with community partners, such as hospitals, clinics, and social service agencies, to provide veterans with comprehensive healthcare and support services. This collaboration will help to ensure that veterans have access to the full range of services they need to address their physical, mental, and social needs.
Conclusion
The expansion of veterans’ healthcare access represents a significant step forward in ensuring that those who have served our nation receive the care they need and deserve. While challenges remain, the initiatives implemented to expand access, improve quality, and enhance efficiency have yielded numerous benefits for veterans and the healthcare system as a whole. By continuing to address the challenges and embrace innovative approaches, we can ensure that veterans have access to the timely, quality healthcare services they need to thrive and live fulfilling lives.