“Mpox Cases Increasing: A Global Health Concern Revisited
Related Articles Mpox Cases Increasing: A Global Health Concern Revisited
- Unifying Threat Intelligence for Enhanced Cybersecurity
- Essential Threat Response Tools for Robust Cybersecurity
- The TikTok Ban Legislation: A Contentious Debate Over National Security, Free Speech, And Economic Interests
- Comprehensive Guide to Anomaly Detection: Preventing Cyber Threats
- Secure Your Endpoints: A Comprehensive Guide to Endpoint Risk Management
Introduction
We will be happy to explore interesting topics related to Mpox Cases Increasing: A Global Health Concern Revisited. Come on knit interesting information and provide new insights to readers.
Table of Content
Mpox Cases Increasing: A Global Health Concern Revisited
Introduction
Mpox, formerly known as monkeypox, is a viral disease that can cause a painful rash, swollen lymph nodes, and fever. While endemic to parts of Central and West Africa, the 2022 global outbreak brought Mpox to the forefront of international health concerns. After a period of decline, recent data indicates a concerning resurgence in Mpox cases, prompting renewed vigilance and public health action. This article will delve into the factors contributing to the increase in Mpox cases, examine the affected populations, discuss the challenges in controlling the spread, and outline the strategies necessary to mitigate this evolving health threat.
Understanding Mpox: Transmission, Symptoms, and Risks
Mpox is caused by the Mpox virus, a member of the Orthopoxvirus genus, which includes the variola virus (the cause of smallpox). The disease is typically transmitted to humans through close contact with infected animals, such as rodents and primates. However, the 2022 outbreak was primarily driven by human-to-human transmission, particularly through close physical contact, including sexual contact.
Transmission:
- Direct Contact: Close physical contact with Mpox lesions, scabs, or body fluids of an infected person.
- Respiratory Secretions: Prolonged face-to-face contact with an infected person can spread the virus through respiratory droplets.
- Contaminated Materials: Contact with contaminated items such as clothing, bedding, or surfaces that have been touched by an infected person.
- Vertical Transmission: Transmission from a pregnant person to their fetus is possible, although rare.
Symptoms:
The incubation period for Mpox typically ranges from 5 to 21 days. Initial symptoms may include:
- Fever
- Headache
- Muscle aches
- Backache
- Swollen lymph nodes
- Exhaustion
A characteristic rash usually develops within one to three days after the onset of fever. The rash progresses through several stages:
- Macules: Flat, discolored spots
- Papules: Raised bumps
- Vesicles: Fluid-filled blisters
- Pustules: Pus-filled blisters
- Scabs: Crusts that form as the lesions heal
The rash often starts on the face and then spreads to other parts of the body, including the hands, feet, and genitals. Lesions can be extremely painful and may lead to complications such as secondary bacterial infections, scarring, and, in rare cases, pneumonia or encephalitis.
Risk Factors:
Certain populations are at higher risk of contracting Mpox or experiencing severe outcomes:
- Men who have sex with men (MSM): The 2022 outbreak disproportionately affected MSM, particularly those with multiple sexual partners.
- People with weakened immune systems: Individuals with HIV/AIDS, organ transplant recipients, and those undergoing chemotherapy are more vulnerable to severe Mpox infections.
- Children: Although rare, children can contract Mpox and may experience more severe symptoms.
- Healthcare workers: Healthcare professionals who are exposed to infected patients without proper protective equipment are at risk.
The 2022 Global Outbreak: A Retrospective Look
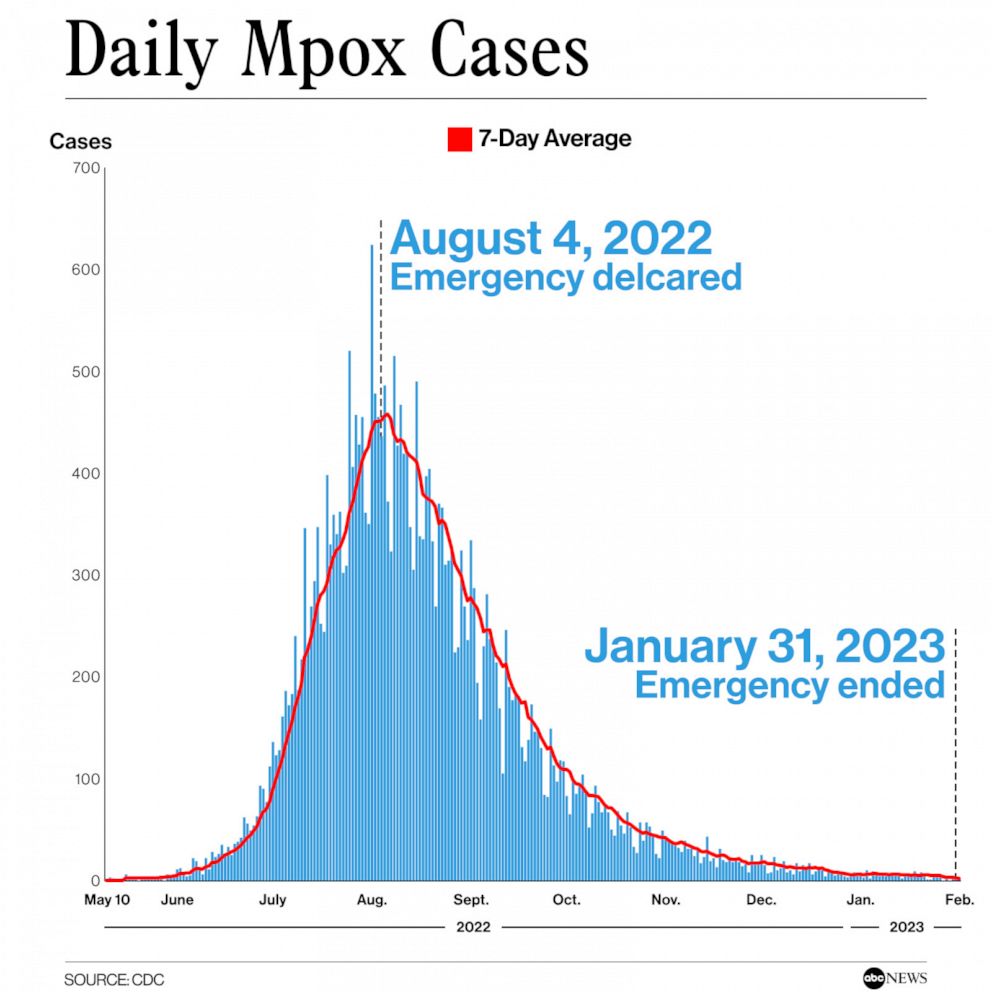
The 2022 Mpox outbreak was unprecedented in its global reach. Prior to this, Mpox cases were primarily confined to certain regions of Africa. The outbreak began in May 2022, with cases reported in Europe, North America, and Australia. The World Health Organization (WHO) declared Mpox a Public Health Emergency of International Concern (PHEIC) in July 2022, highlighting the urgency of the situation.
The rapid spread of Mpox during the 2022 outbreak was attributed to several factors:
- Increased International Travel: The resumption of international travel following the COVID-19 pandemic facilitated the spread of the virus across borders.
- Close Contact at Mass Gatherings: Large social events and gatherings, particularly those involving close physical contact, contributed to transmission.
- Lack of Awareness: Limited awareness of Mpox symptoms and transmission routes among the general public and healthcare providers hindered early detection and prevention efforts.
- Stigma and Discrimination: Stigma associated with Mpox, particularly within the MSM community, led to underreporting of cases and delayed access to healthcare.
The Resurgence of Mpox Cases: Contributing Factors
While the global Mpox outbreak appeared to be waning in late 2022 and early 2023, recent data indicates a concerning resurgence in cases in various regions around the world. Several factors may be contributing to this increase:
-
Waning Immunity: The immunity conferred by vaccination or previous infection may be waning over time, making individuals more susceptible to Mpox.
-
Relaxation of Preventive Measures: As the initial wave of the outbreak subsided, some individuals and communities may have become less vigilant about preventive measures such as vaccination, safe sexual practices, and avoiding close contact with infected individuals.
-
New Variants: The emergence of new variants of the Mpox virus could potentially be more transmissible or cause more severe disease, although further research is needed to confirm this.
-
Underreporting and Surveillance Gaps: Inadequate surveillance systems and underreporting of cases may be masking the true extent of the resurgence.
-
Access to Healthcare: Barriers to accessing healthcare, including stigma, discrimination, and lack of insurance, may prevent individuals from seeking timely diagnosis and treatment.
-
Complacency: The perception that Mpox is "over" may lead to complacency among healthcare providers and public health officials, resulting in delayed or inadequate responses to new outbreaks.
Affected Populations: Who is at Risk?
While Mpox can affect anyone, certain populations remain at higher risk:
- MSM: Men who have sex with men continue to be disproportionately affected by Mpox, particularly those with multiple sexual partners or those who engage in anonymous sex.
- People with HIV/AIDS: Individuals with HIV/AIDS are more likely to experience severe Mpox infections and complications.
- Immunocompromised Individuals: People with weakened immune systems due to other medical conditions or treatments are also at increased risk.
- Children: Although rare, children can contract Mpox and may experience more severe symptoms.
- Healthcare Workers: Healthcare professionals who are exposed to infected patients without proper protective equipment are at risk.
Challenges in Controlling the Spread of Mpox
Controlling the spread of Mpox presents several challenges:
- Limited Vaccine Supply: The global supply of Mpox vaccines is limited, making it difficult to vaccinate all at-risk individuals.
- Vaccine Hesitancy: Vaccine hesitancy and misinformation can hinder vaccination efforts.
- Stigma and Discrimination: Stigma associated with Mpox can lead to underreporting of cases and delayed access to healthcare.
- Lack of Awareness: Limited awareness of Mpox symptoms and transmission routes among the general public and healthcare providers can hinder early detection and prevention efforts.
- Surveillance Gaps: Inadequate surveillance systems can make it difficult to track the spread of the virus and identify new outbreaks.
- Animal Reservoirs: The presence of animal reservoirs of the Mpox virus in Africa poses a long-term challenge to eradication efforts.
Strategies to Mitigate the Resurgence of Mpox
To effectively mitigate the resurgence of Mpox, a multi-pronged approach is needed:
-
Vaccination: Prioritize vaccination of at-risk populations, including MSM, people with HIV/AIDS, and healthcare workers. Ensure equitable access to vaccines and address vaccine hesitancy through targeted education and outreach.
-
Testing and Diagnosis: Improve access to Mpox testing and diagnosis, particularly for individuals with suspected symptoms. Implement rapid diagnostic tests to facilitate early detection and isolation of cases.
-
Treatment: Provide timely access to antiviral treatments for individuals with severe Mpox infections.
-
Public Health Education: Conduct public health education campaigns to raise awareness of Mpox symptoms, transmission routes, and prevention measures. Target messaging to at-risk populations and address stigma and discrimination.
-
Surveillance and Monitoring: Strengthen surveillance systems to track the spread of the virus and identify new outbreaks. Implement genomic surveillance to monitor for the emergence of new variants.
-
Contact Tracing: Conduct thorough contact tracing to identify and monitor individuals who may have been exposed to Mpox.
-
Community Engagement: Engage with affected communities to build trust and ensure that prevention and control efforts are culturally appropriate and effective.
-
Global Collaboration: Strengthen global collaboration to share information, resources, and expertise to combat Mpox. Support research to develop new vaccines, treatments, and diagnostic tools.
Conclusion
The resurgence of Mpox cases is a concerning reminder that this viral disease remains a significant global health threat. To effectively mitigate the resurgence, a comprehensive and coordinated response is needed, including vaccination, testing, treatment, public health education, surveillance, contact tracing, community engagement, and global collaboration. By working together, we can control the spread of Mpox and protect vulnerable populations from this debilitating disease. It is crucial to maintain vigilance, address stigma, and ensure equitable access to healthcare to prevent future outbreaks and safeguard public health.